- Slug: BC-CNS-Opioids Alternatives,2350
- Photos available (thumbnails, captions below)
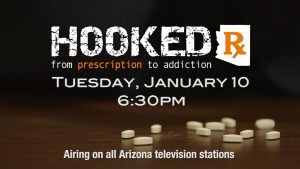
- EDS: PLEASE RUN THE HOOKED PROMO PHOTO (below) OR THIS BOX WITH THIS STORY IF YOU PLAN TO PUBLISH PRIOR TO JAN. 10: Watch “Hooked Rx: From Prescription to Addiction,” a 30-minute commercial-free investigative report airing at 6:30 p.m. on Jan. 10 on 30 broadcast TV stations in Phoenix, Tucson and Yuma and 97 of the state’s radio stations. For the full report, go to hookedrx.com.
PHOENIX – Eric Johnson has had pain throughout his life.
At 8, doctors diagnosed him with mononucleosis – also known as the kissing disease. That likely led to fibromyalgia, a common chronic pain disorder affecting muscles and soft tissues, as an adult, he said.
In 2011, he had such extreme breathing difficulties that he went to the emergency room in Tucson, where doctors discovered he had myasthenia gravis, a disease that weakens the muscles.
Johnson, 65, also underwent open chest surgery for a cancerous thymus gland.
At one point, the Phoenix resident was “in such extreme pain, I wanted to kill myself.”
The pain felt like being beaten with sticks all over the body, “not so much as it’s happening, but when it’s over, the ache, that pain’s everywhere,” he said.
Johnson has taken pain relievers, such as Lyrica and tramadol, as well as opioids, such as morphine and oxycodone. But he prefers medical marijuana, which he says has helped reduce the amount of prescription pills he has to take.
Johnson said he’s worried about getting hooked on prescription drugs. He wanted to wait as long as possible before taking opioids because “when the pain gets so bad, there’s no alternative, only increased dosages or stronger prescriptions offer some relief.”
Nearly 40 million adults in the U.S. suffer from severe pain, according to the National Institutes of Health. Chronic pain, as opposed to acute pain, can last months to years. Acute pain, on the other hand, lasts less than six months and is directly related to tissue damage.
To treat chronic pain, doctors generally prescribe opioids. In 2012 alone, doctors wrote 259 million prescriptions for painkillers, according to the Centers for Disease Control and Prevention.
But opioids are addictive and even deadly. More than 14,000 people in the U.S. died from prescription opioid overdoses in 2014 – that’s nearly 40 people a day, according to the CDC.
Bentley Bobrow, medical director of the Bureau of Emergency Medicine and Trauma Services at the Arizona Department of Health Services, said both patients and doctors are approaching the opioid and chronic pain problems with the wrong treatments and attitudes.
“People are accustomed to going to a doctor and getting a pill,” Bobrow said. “And for a lot of health care providers, that’s sort of all they know. Back pain, pain pills. Neck pain, pain pills. Abdominal pain, pain pills. Some of it is the medical profession’s fault, but some of it is also that for the last couple of years, we’ve been taught that pain pills are good.”
The CDC released new guidelines for prescribing opioids for chronic pain in May. They caution doctors to consider the risks of opioid pain medication and provide 12 recommendations to best treat chronic pain, including using non-pharmacologic and non-opioid therapy and establishing treatment goals.
“We’ve treated people who have chronic pain with opioids for a long time, and inadvertently, we’ve habituated a lot of patients. Now we have a huge related public health problem of opioid overuse, abuse and even overdose,” Bobrow said. “The challenge is to have health care providers and patients understand how chronic pain works and especially how they can manage themselves with alternative techniques.”
Some health professionals and patients have turned to other strategies, including medical marijuana, epidurals, stretching therapy, acupuncture, cognitive behavioral therapy, mindfulness and yoga. However, these methods also have limitations and disadvantages. Here’s a closer look at some alternative treatments:
Medical marijuana
WHAT IT DOES: Federal restrictions have hampered research on marijuana’s potential to treat chronic pain, but many users vow that it works.
Medical marijuana dispensaries in Arizona sell it in various forms, including edibles, concentrates, topical creams and vapors.
Elaine Burns, a naturopathic medical doctor at the Southwest Medical Marijuana Evaluation Center in Scottsdale and Phoenix, said since Arizona voters legalized medical marijuana in 2010, marijuana has alleviated her patients’ pain or worked with other medication to lower the pain.
They “forget that they had pain,” she said.
PROS: According to a 2006 study on the role of cannabis in pain control, researchers indicated that one compound found in medical marijuana is effective in treating pain, depression, appetite and memory.
“I like feeling better and (medical marijuana) helps me feel better,” Johnson said. “Medical marijuana helps tremendously with my attitude about life.”
The majority of Burns’ patients come in with the goal of getting off prescription opioids.
“Cannabis is demonstrating they tried other therapies that haven’t worked and now want to try using cannabis for chronic pain,” Burns said.
CONS: Bobrow doesn’t recommend using medical marijuana as an alternative. The science behind cannabis is still new, he said.
“You’re still swapping out one drug for another drug, and you’re not really approaching or attacking the central part of the problem,” he said. “You’re just masking it with a drug, and marijuana is not a completely innocuous drug. It does have side effects.”
Because the U.S. Drug Enforcement Administration still classifies marijuana as a Schedule 1 drug, which means it has no medical benefits and has a high potential for abuse, there haven’t been many scientific studies proving its medical use.
But Burns said the side effects of medical marijuana, including anxiety, paranoia, agitation, red eyes, dry mouth and increased appetite, are not life-threatening.
Gene Herman, a chronic pain patient from Peoria, said he is wary of medical marijuana because of the legality. Despite medical marijuana being legal in Arizona, he doesn’t want to risk it since it is still against federal law.
“Until everything’s all straightened out nationwide, as far as rules and regulations and laws, the last thing I’d want to do is be a bad example for my grandkids or something like that,” he said. “Not to mention my wife would kill me.”
Epidurals
WHAT IT DOES: Epidurals are steroid treatments injected to decrease pain and inflammation caused by a herniated disc, sciatica or spinal stenosis.
PROS: Epidural injections are one of the most commonly used methods to manage chronic spinal pain, according to a 2007 study. The study found epidural injections effective for short-term relief.
“It can give people benefits, particularly for those who have acute pain,” Bobrow said.
CONS: The effects are limited for long-term relief or chronic pain.
Bobrow said epidurals work on the peripheral nervous system, not the central nervous system, where chronic pain is felt. The science is also lacking, he said.
“The science behind epidurals for chronic pain isn’t overwhelming. Lots and lots of people get epidurals for chronic pain, but they don’t get better,” he said. “A lot of pain is felt in the central nervous system, the brain, and epidurals work on the peripheral nervous system.”
Stretching therapy
WHAT IT DOES: Stretching therapy targets muscles, joints and bones to decrease pain and maximize blood flow.
Herman said his pain began when he was a construction worker for the U.S. Department of Energy. When climbing a power tower in 2004, Herman stumbled on a platform. After going to the emergency room, Herman went to the Pain Center of Arizona and learned he had two herniated discs.
Herman treats the pain with a combination of stretching therapy, epidurals and hydrocodone, an opioid.
PROS: “When people are stretching, they’re doing exercise, they’re gaining confidence,” Bobrow said. “There’s a very therapeutic aspect in stretching, exercise and natural endorphins.”
Herman said he doesn’t believe he will have to increase his hydrocodone dosage, mostly because of his lifestyle and the way he’s taking care of himself physically, by stretching.
“Even before I do anything in the morning, I must spend 10 minutes in bed just stretching my legs and lower back before I get up,” Herman said. “And I do that religiously.”
If he feels a twinge of a nerve through the course of the day, he will stop to stretch, he said.
CONS: There’s not much risk in stretching therapy, Bobrow said, as long as people are stretching within their own limits.
However, one 2012 study indicated that although stretching may work for certain types of pain, it may not work for all injuries.
Acupuncture
WHAT IT DOES: Acupuncture, the Chinese practice of inserting thin needles into a patient’s skin at certain points, is a common alternative in treating pain.
Acupuncture can release neurotransmitters and chemicals involved in pain, said Lonnie Zeltzer, director of a pain clinic at the University of California Los Angeles and member of the Institute on Medicine.
Traditional Chinese medicine stresses the flow of energy or life force, also known as chi, in the body. To treat pain, acupuncture practitioners insert needles in the body to regain energy balance.
PROS: Although there is contention between the methods of acupuncture and whether acupuncture is effective for chronic pain, research published in the Archives of Internal Medicine indicated acupuncture relieved pain by about 50 percent. The research looked at 29 studies, which included nearly 18,000 patients.
“Acupuncture is effective for the treatment of chronic pain and is therefore a reasonable referral option,” the study concluded. “Significant differences between true and sham acupuncture indicate that acupuncture is more than a placebo.“
CONS: Although acupuncture is effective for many people, it may not work for those who don’t believe in it.
“It’s much more likely to work, with acupuncture, if you believe in it and it’s more likely to help you,” Bobrow said.
A 2002 study reviewing clinical acupuncture trials notes that “clearly there are too few trials of sufficient quality and homogeneity” to draw conclusions about treating chronic pain.
Non-addictive pain relievers
WHAT IT DOES: Scientists have worked for years to develop non-addictive medicines that can still relieve chronic pain. Gavril Pasternak, a researcher at the Memorial Sloan Kettering Cancer Center, said the research field has been “moving quickly” to develop safer opioids.
“For the first time in decades, we may be seeing new chemical entities being developed as potent painkillers,” he wrote in an email. “A lot of things are changing.”
At the University of Arizona, researchers have developed a non-addictive pain reliever that could be available in 10 to 15 years.
Alexander Sandweiss has conducted research on opioid receptors and the “reward pathway” at the University of Arizona’s Department of Pharmacology to develop the compound.
The pain reliever works to turn on opioid receptors in the body to stop pain and stops addiction by blocking a specific receptor called neurokinin 1, Sandweiss said.
PROS: These types of pain relievers could prevent people from getting addicted to opioids in the first place, Sandweiss said.
CONS: Compounds must go through several trials and steps before human patients can use them. Less than a percent of compounds that work in animals also end up working in humans, Sandweiss said.
And, this compound would not necessarily be targeted to patients like Eric Johnson or Gene Herman, who suffer from chronic pain and already take opioids. Rather, it’s for those who want to inhibit their pain, but don’t want to take opioids in the first place.
Cognitive behavioral therapy
WHAT IT DOES: Cognitive behavioral therapy is a form of psychotherapy that changes the patterns of thinking or behavior, therefore changing the way patients feel.
Emotions and pain are connected, Bobrow said.
“We know that when people anticipate pain, it’s much, much worse,” Bobrow said. “When we’re not anticipating or paying attention to pain, the pain experience is far less so in these cognitive therapies, people can learn very quickly and effectively how to manage their anticipation of pain and to not heighten pain.”
PROS: A study at the University of Washington on cognitive behavioral therapy for those with chronic pain calls the method the “gold standard” of psychological treatments.
Cognitive behavioral therapy also does not have the risks of chronic pain medications, surgeries and other interventional methods.
CONS: Although the study notes the therapy’s effectiveness, most patients with chronic pain never receive it, the study concluded. Although it’s often integrated into medical settings, cognitive behavioral therapy needs to be expanded, especially in primary care, the study said.
Professionals must improve their knowledge of the treatment and the competence of therapists administering the therapy, the study said.
Mindfulness meditation
WHAT IT DOES: Chronic pain patients can ease their pain through mindfulness meditation, focusing on a single sense, such as breathing.
PROS: When patients practice mindfulness meditation, their pain and function improve, Bobrow said.
“They don’t just hurt less, they can do more,” Bobrow said. “And part of the way that works is that oftentimes, our minds get active, sometimes overactive. That actually exacerbates pain, and people can learn to calm down and quiet their mind. When people actually learn to calm down their minds, their pain is far better. Sometimes, it even completely goes away.”
A study conducted at Wake Forest University showed that some people could reduce their pain by 40 percent using mindfulness meditation.
CONS: According to a Harvard Medical School presentation on meditation, many health care plans don’t cover the cost of mindfulness meditation. However, many insurance companies offer discounts for fitness programs.
Yoga
WHAT IT DOES: Chronic pain patients can help relieve their pain through yoga by combining yoga poses and conscious breathing.
PROS: “It’s both the combination of the physical aspect of yoga, the movement is helpful, but also the emotional and psychological part,” Bobrow said. “Yoga is very meditative and helps calm the mind. It also builds confidence. … When people feel confident, they feel better.”
According to a study in the Annals of Internal Medicine that surveyed 313 people with chronic pain, weekly yoga increased their mobility more than the standard medical care for the chronic lower back pain.
CONS: There is little research for the mechanisms of yoga that relieve back pain, since it involves both physical movement and mental focus, according to a study comparing yoga, exercise and a self-care book for chronic pain.
Cronkite News reporter Kate Peifer contributed to this article.
^__=